Nursing Homes Have a Long History of Infection Control Problems, Says Government Report
According to a report released by the U.S. Government Accountability Office in 2020, 82% of all nursing facilities across the U.S. have suffered from some level of infection control deficiency between 2013-2017, with nearly half of those cited for “persistent problems” in controlling infection at the facility for multiple consecutive years.
Vohra Wound Physicians, the leader in post-acute wound care, is adamant regarding the importance of infection control to prevent disease spread in nursing homes and senior care centers as an essential skill that every facility and healthcare provider should have and practice every day.
The report in question was commissioned to examine infection prevention and control shortcomings in U.S. nursing homes prior to the COVID-19 pandemic, assess the quality of federal oversight protocols, and gauge nursing homes’ emergency preparedness procedures in response to emerging infectious diseases—both now and in the future.
There are currently about 15,500 nursing homes in the United States. The report was based on data collected from all 50 states, including the District of Columbia, and the findings report that every single state contained nursing homes that had been cited for multiple consecutive years for failure to meet infection control standards.
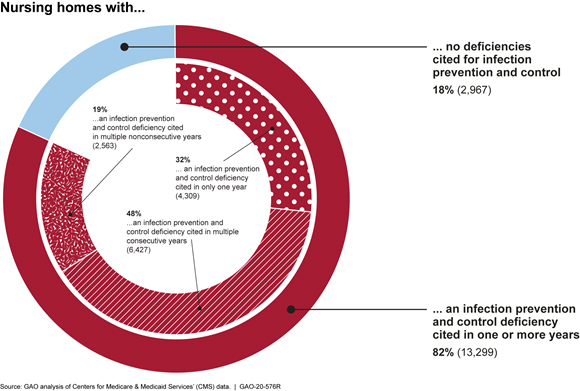
Specifically, the report found that among all nursing homes, failure to follow procedures to prevent and control infection was widespread and often these deficiencies were found over multiple years.
The most common type of infection control infractions that were cited among nursing and healthcare staff include poor hand hygiene and a lack of proper infection preventive measures—like isolating sick patients and using personal protective equipment—to manage disease outbreaks at the facility.
However, the report also points out that 99% of the infection control and prevention deficiencies found in that time period were classified as “not severe,” which also meant that in the majority of instances, the senior care facility did not receive any type of enforcement actions from the Centers for Medicare and Medicaid Services, the entity responsible for ensuring nursing facilities across the nation, have proper health and safety measures in place for staff and patients.
The recent pandemic and the fact that nursing homes continue to be “hot spots” for disease spread among patients and staff (it’s estimated that one third of all COVID-19-related deaths have occurred in a nursing home) have raised concerns about the overall health and safety procedures—infection prevention and control in particular—in place at these facilities in order to keep nursing staff and patients alike safe from increased disease spread.

Best Practices for Nurses to Prevent Wound Infection
Skilled nursing staff are responsible for following strict infection control and prevention procedures, not only to protect the patient population from disease spread but also to protect themselves from exposure and infection. If you work in a nursing home facility or with elderly patients in a home healthcare setting, remember the following:
Infection Control Checklist
- Always use Universal Precautions, which means treating every bodily fluid as if it was infectious.
- Wash hands before and after patient contact, every time.
- Use clean gloves with each new patient and between dressing removal prior to any procedure.
- Replace gloves if you suspect they have been contaminated.
- Once you wear gloves, do not reach into your pockets and keep non-patient contact to a minimum.
- Use the proper personal protective equipment for the situation (e.g. face masks, gowns, respirators, etc.).
- When examining patients, move from least potentially contaminated area to most (not the reverse).
- Discard of disposable instruments (e.g. sharps) at the point of patient contact—don’t remove and dispose of elsewhere.
- Sufficiently clean any non-disposable instruments between uses, up to or beyond local standards (e.g. use alcohol swabs to clean the
bell of your stethoscope). - Minimize patient contact with non-disposable items when possible (e.g. keep computer on a cart).
- Do not place items directly on patients’ furniture or surfaces (e.g. bed, dresser, table) without a protective barrier.
Nursing homes and senior care centers must ensure the safety of patients by prioritizing infection control procedures, starting with educating nurses, physicians, healthcare workers and patients on the facility’s infection prevention protocol—and working to gain compliance within the facility.

Vohra is the leader in post-acute wound care, providing both bedside and telemedicine wound care treatment and management solutions to nurses, physicians, Skilled Nursing Facilities and patients. Learn how Vohra is setting the standard in the new world of healthcare here.
Make a Difference in
Patients' Lives and
Your Own Career
JOIN VOHRA WOUND CAREStay up to date on the latest in wound care.
Join our mailing list today!

Thank You For Successfully Registering!
Stay tuned for the latest news and treatments in wound care tailored for medical professionals like you.
