18 Ways to Die: Antibiotic Resistance. The Crisis is Now.
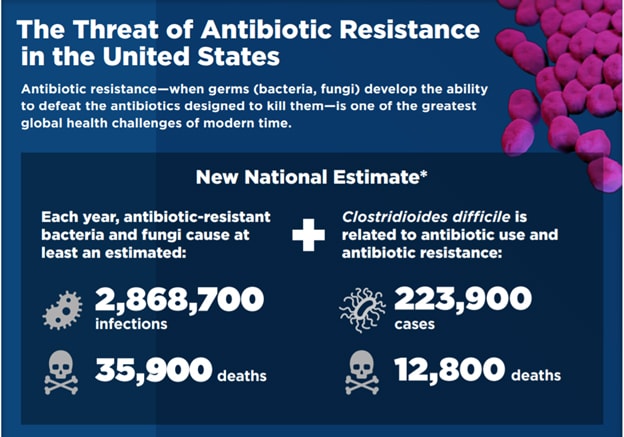
35,000 people will die from antibiotic-resistant infections in the US this year, while another 2.8 million will fight an antibiotic-resistant infection. The rise of antibiotic resistance has been widely discussed and many articles have been written about the subject. Just a few months ago, I reviewed the emerging threat of Candida auris.
The Centers for Disease Control and Prevention (CDC) recently released its second-ever report on the threats of antibiotic resistance, updating its seminal 2013 report.
The 2019 report has good news and some potential bad news. One of the concerning findings is that there are 18 threats that the CDC has broken down into 3 categories. The CDC lists five urgent, eleven serious, two concerning plus three more on a “watch list.” The good news is that the focus over the last few years on reversing the trend in resistance has helped. Deaths from drug-resistant infections have reduced 18% from 2013. The threat remains, though and is very real and demands our focus to increase. Dr. Redfield, the current CDC director, made a very important point in this report when he said, “Stop believing that antibiotic resistance is a problem ‘over there’ in someone else’s hospital, state, or country—and not in our own backyard. Antibiotic resistance has been found in every U.S. state and in every country across the globe. There is no safe place from antibiotic resistance, but everyone can take action against it. Take action where you can, from hand-washing to improving antibiotic use.”
Hand hygiene should be thought of as a before and after the event. Some minimum points are before and after putting on gloves, before and after contact with patients, before and after wound care, before and after contact with innominate objects near the patient. A useful instructional video has been produced by the Centers for Medicare and Medicaid Services on how to wash your hands properly.
EDITOR’S NOTE: Vohra Wound Physicians are on the front lines in combatting and stopping the spread of antibiotic resistance. If you are a physician, driven to make a difference, click here and join Vohra today!
The CDC’s list of the 18 that might kill you and the 3 to watch are:
Urgent Threats
- Carbapenem-resistant Acinetobacter
- Candida auris (C. auris)
- Clostridioides difficile (C. difficile)
- Carbapenem-resistant Enterobacteriaceae (CRE)
- Drug-resistant Neisseria gonorrhoeae (N. gonorrhoeae)
The urgent threats result in a wide range of cases each year from a few hundred cases of C. Auris to the over half a million cases of Neisseria gonorrhoeae. Each is significant and affects various populations. Clostridioides difficile causes over 12,000 deaths each year and is commonly found in patients in long-term care facilities.
Some encouraging findings show that the incidence of infections in the 65 years old plus populations has decreased, and this is linked to a decreased use of fluoroquinolones in this population. Proper handwashing with soap and water instead of alcohol hand gels and other stewardship practices has also helped.
Serious Threats
- Drug-resistant Campylobacter
- Drug-resistant Candida
- Extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae
- Vancomycin-resistant Enterococci (VRE)
- Multidrug-resistant Pseudomonas aeruginosa (P. aeruginosa)
- Drug-resistant nontyphoidal Salmonella
- Drug-resistant Salmonella serotype Typhi
- Drug-resistant Shigella
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Drug-resistant Streptococcus pneumoniae (S. pneumoniae)
- Drug-resistant Tuberculosis (TB)
Concerning Threats
- Erythromycin-resistant group A Streptococcus
- Clindamycin-resistant group B Streptococcus
Watch List
- Azole-resistant Aspergillus fumigatus (A. fumigatus)
- Drug-resistant Mycoplasma genitalium (M. genitalium)
- Drug-resistant Bordetella pertussis (B. pertussis)
The Center of Excellence in Wound Management was created by Vohra Wound Physicians in order to highlight and identify facilities that have developed a superior wound management program. It is a yearly distinction and the facility must meet all criteria:
- Less than 1% wound related hospitalization rate
- Vohra wound physician rounding with an average wound census of more than 5 patients per week
- Regular team meetings with a focus on Quality and Process Improvement (QAPI)
- Designated Vohra wound care certified nurse with availability 7 days a week
Antibiotic resistance at its simplest is antibiotic use and the spread of microbial infections. Manage both of these effectively, and we can slow or ever stop resistance. New antibiotics will help but will not be the solution.
Pew Trusts reports that currently, only 42 antimicrobial drugs targeted at addressing resistance are in development, and of these, just 8 or 9 will ever make it to market. It is our duty as healthcare providers, patients, and family members to practice antibiotic stewardship in every setting and in our daily activities.
Reduce the improper use of antibiotics, antimicrobials (plain soap works just fine we don’t need to use antimicrobial augmented products routinely), demand our food supply stop improper use of antimicrobials (commonly used as growth agents, and fungicides). In 2016 nearly 14 million kilograms of antibiotics were used in the United States in the production of cattle, pigs and chickens, and starting in 2017, use now requires veterinary oversight and much work remains. That is the equivalent of every single person in the United States being prescribed tetracycline twice a day for 40 days.
I use that to illustrate how systemic and pervasive antibiotic use has become and remind us that antibiotic resistance is not just a medical problem; it is also a food supply and environmental issue. The key to our future and to continued progress is three-fold: it is preventing infections, improving antibiotic use (right drug, right dose, right duration), and stopping the spread of resistance when it does occur.
The threat affects every one of us and the solution involves each of us. This is why the CDC’s One Health directive recognizes our health, the health of animals, and the environment are all interconnected. Take steps today to ensure the next report on resistance has less ways to die a reduction in emerging threats.
Make a Difference in
Patients' Lives and
Your Own Career
JOIN VOHRA WOUND CAREStay up to date on the latest in wound care.
Join our mailing list today!

Thank You For Successfully Registering!
Stay tuned for the latest news and treatments in wound care tailored for medical professionals like you.
